Scientific Program

Dr. Luigi Vetrugno
Department of Medicine, University of Udine, Italy.
Biography:
Dr. Luigi Vetrugno is an emergency consultant at the Department of Medicine, in the University of Udine, at the University-Hospital of Friuli Centrale, Udine, Italy.
Abstract
Keywords: Consensus, Coronavirus disease 2019, Intensive care, Lung ultrasound.
Introduction:
The use of lung ultrasound (LUS) in the intensive care set- ting has increased during the coronavirus disease 2019 (COVID-19) pandemic. It is being employed as a diagnostic and monitoring tool in patients with COVID-19- related pneumonia a condition which in some cases evolves into acute respiratory distress syndrome (ARDS) [1]. Lung ultrasound presents many advantages over other imaging techniques: it is readily available at the bedside, thus avoiding the need to transport patients to the radiology department, and it is radiation-free and highly repeatable, making it suitable for lung monitoring purposes [2]. Lung damage in COVID-19 pneumonia is mainly localized to the peripheral regions of the lungs, thus easily accessible to ultrasound [3]. The sensitivity and negative predictive value of LUS for COVID-19 pneumonia are both higher compared with those for chest X-ray [4]. Moreover, many studies show a close correlation between LUS and computed tomography (CT) scan findings [5]. Given the prolonged need for mechanical ventilation in COVID-19 and long intensive care unit (ICU) stay, repeated lung assessments are usually required. CT remains the reference imaging technique or lung assessment, but it is unsuitable as a monitoring tool due to its use of ionizing radiation. It also necessitates patient contact with healthcare providers outside the ICU, increasing the opportunity for this highly infectious disease to spread. The quantitative evaluation of lung disease by means of the LUS score provides a reliable method for assessing lung aeration in both ARDS and COVID-19, and may further help in monitoring lung recovery and in the daily optimization of ventilation strategies (i.e., positive end- expiration pressure [PEEP] titration, and the use of prone positioning) [6]. Finally, LUS permits the early bedside detection of complications, such as pneumothorax [7] and ventilator-associated pneumonia [8]. As a consequence, LUS has earned a leading position in the management of COVID-19 patients, being a reliable, time-sparing, and easy-to-learn alternative to traditional imaging techniques [9, 10]. However, the recent literature is mainly focused on its applications within the Emergency Department [11]. Although Canadian Internal Medicine Ultrasound (CIMUS) experts recently established their recommendations for medical inpatients with COVID-19 [12], consensus guidelines dedicated to COVID-19 ICU patients and officially acknowledged by a national intensive care scientific society are lacking. To fill this gap, we aimed to produce an expert consensus on the bedside use of LUS in critically ill COVID-19 patients by a national panel of anaesthesiology and intensive care physicians.
Methods:
Consensus process design
This project was conducted according to a modified Del- phi method to reach consensus on key aspects of the use of LUS in critically ill patients with COVID-19. Discussions were based on the available scientific evidence as well as the panel of experts’ own clinical experience. The experts were selected by the project coordinators (LV and FM) based not only on their clinical and scientific interest in the topic [13] but also the opinion of intensivists who are not experts in LUS but who understand the context of critically ill COVID patients, and the potential role of lung ultrasound was invited. After an initial (online) kick-off meeting between the coordinators, the panellists, the methodologists (AC and DP), and the evidence review team (MI and DO), the project coordinators proposed a list of the most relevant clinical questions to the whole panel, which was then asked to submit a blind Boolean vote (“agree/disagree on the relevance”) as well as comments and proposals for their modification. In response, the coordinators made the appropriate changes to the clinical questions, which were finally approved by the whole panel through a second round of voting. The coordinators then assigned the work on each clinical question to a designated group of experts, each of which was led by a designated group head (PP, PN, EB, TB, and SM). The list of clinical questions and the final consensus-based statements.
Result:
The panel was composed of a total of 18 experts, 4 methodologists, and 2 senior heads. The panel produced a total of 20 statements. The criteria for a consensus of agreement (i.e., a score in the range 7 - 9 provided by 75% or more of respondents, and a median score value also within this range) were met for 18 out of 20 statements in the first round of voting. Consensus was not achieved in relation to statements no. 5 and no. 17 (see Fig. S 2, Additional file 2). After the second round of voting, consensus of agreement was achieved on all statements. The median score (plus interquartile range) and agreement percentage for all the statements contained in the final consensus report.
FIG 1: The lung ultrasound score (LUS) can be applied to assess the loss of aeration by dividing the thorax into 12 specific regions, six on the right and six on the left in supine or prone position assign each region a score from 0 (normal lung) to 3 (lung consolidation). Anterior, lateral, and posterior fields are identified by sternum, anterior, and posterior axillary lines. The entire examination can be performed without any change in patients position. Score: 0 = normal aeration (A-lines and lung sliding or maximum 2 well-spaced B-lines); score 1 = moderate loss of aeration (> = 3 well-spaced B-lines with lung sliding, coalescent B-lines/sub pleural consolidations occupying < 50% of the pleural line); score 2 = severe loss of aeration (> = 3 well-spaced B-lines with lung sliding, coalescent B-lines/sub pleural consolidations occupying clearly > 50% of the pleural line); score 3 = complete loss of aeration:lobar/hemi lobar consolidation with predominant tissue like pattern which will lead the patient into critical condition. 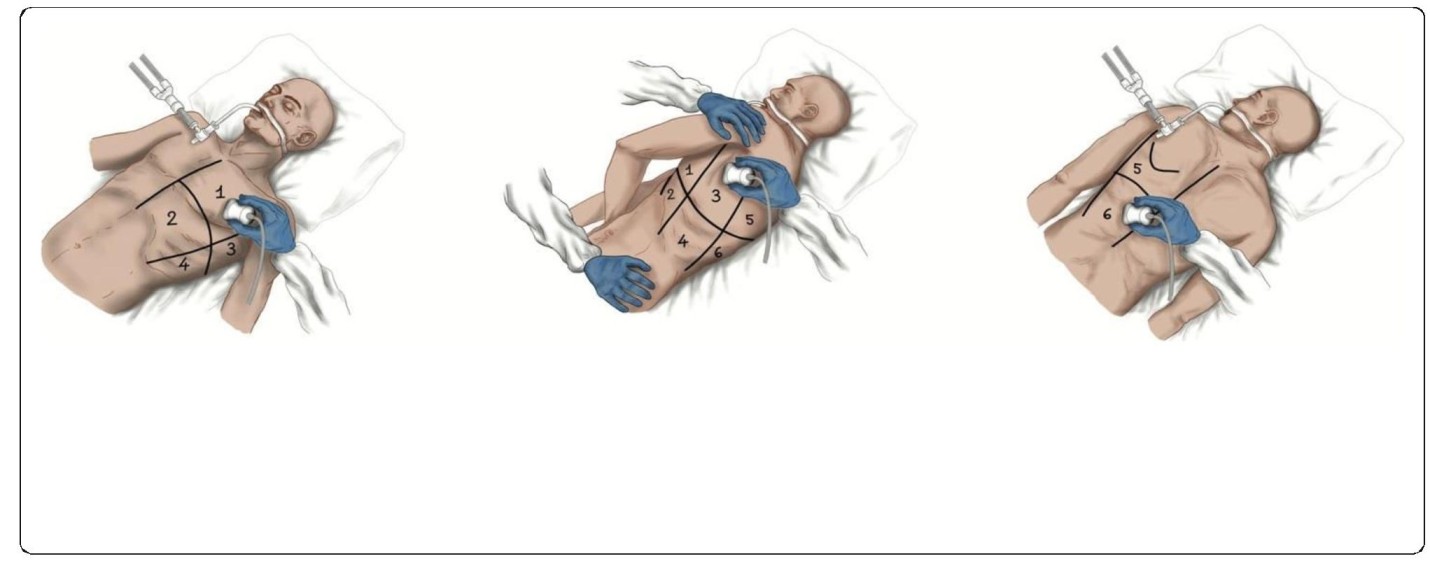
Conclusion:
The Lung Ultrasound Working Group of the Italian Society of Analgesia, Anaesthesia, Resuscitation, and Intensive Care produced 20 consensus statements on the use of lung ultrasound in COVID-19 patients admitted to the ICU. This expert consensus strongly suggests integrating lung ultrasound findings in the clinical management of critically ill COVID-19 patients.
- Emergency Medicine
- Personalized Medicine
- Critical Care Nursing
- Intensive Care Unit
- Cardiac Emergencies
- Pediatric Emergencies
- Medical Toxicology
- Critical Care & Anaesthesiology
- Critical Care or Intensive Care Medicine
- Emergency Drugs and Its Administration

