Scientific Program
Keynote Session:
Oral Session 1:
- Poly-addiction and dual pathology: Concepts and debates
Title: Poly-addiction and dual pathology: Concepts and debates
Biography:
Jaouad Saidi is a Researcher in Clinical Psychology & Integrative Psychopathology in Children, Teens, Adults and Senior, he is also a part of FLDM - Fez - Faculty of Letters and Human Sciences, Morocco.
Abstract:
This study was interested in exploring the nature of the interaction between the two psychiatric and addiction components in the same individual from a clinical perspective. The general objective of this study was to determine the polyconsumption of psychoactive substances in psychiatric patients. Does psychiatric pathology fuel addictions to psychoactive substances? Does addiction to psychoactive substances fuel psychiatric pathology? The study described and based on the screening of psychiatric patients with possibly associated addictive disorders. These patients were chosen as adults (24-54 years old) within the CHU-Fes (MOROCCO). We report five clinical cases with dual pathology; psychiatric disorder and Poly-addictions. Each patient who has been diagnosed by psychiatrist - addictologists. The assessment consists primarily of clinical observation and several semi-structured interviews. We also used the M.I.N.I. (DSM-IV) for screening. On the other hand, we used the addictive pathology test (DSM-V). We have also used various measurement and verification tools and instruments, such as the CAST test for the evaluation of the degree of addiction in the context of cannabis consumption, and the test (Fagerstrom) for the evaluation of the problematic tobacco use, and finally we used the AUDIT test, for the detection of problematic alcohol use. This study led us to see these psychiatric people consuming products, the results of this most prominent comorbidity in them in relation to their mechanisms, addiction becomes like the product of the interaction between psychological precursors and addictive processes. This duality is poorly understood but in reality frequent, would lead to pathological multiple consumption of the product. The importance of paying particular attention to the issue of dual diagnosis, the two components, for the deployment of their appropriate care.
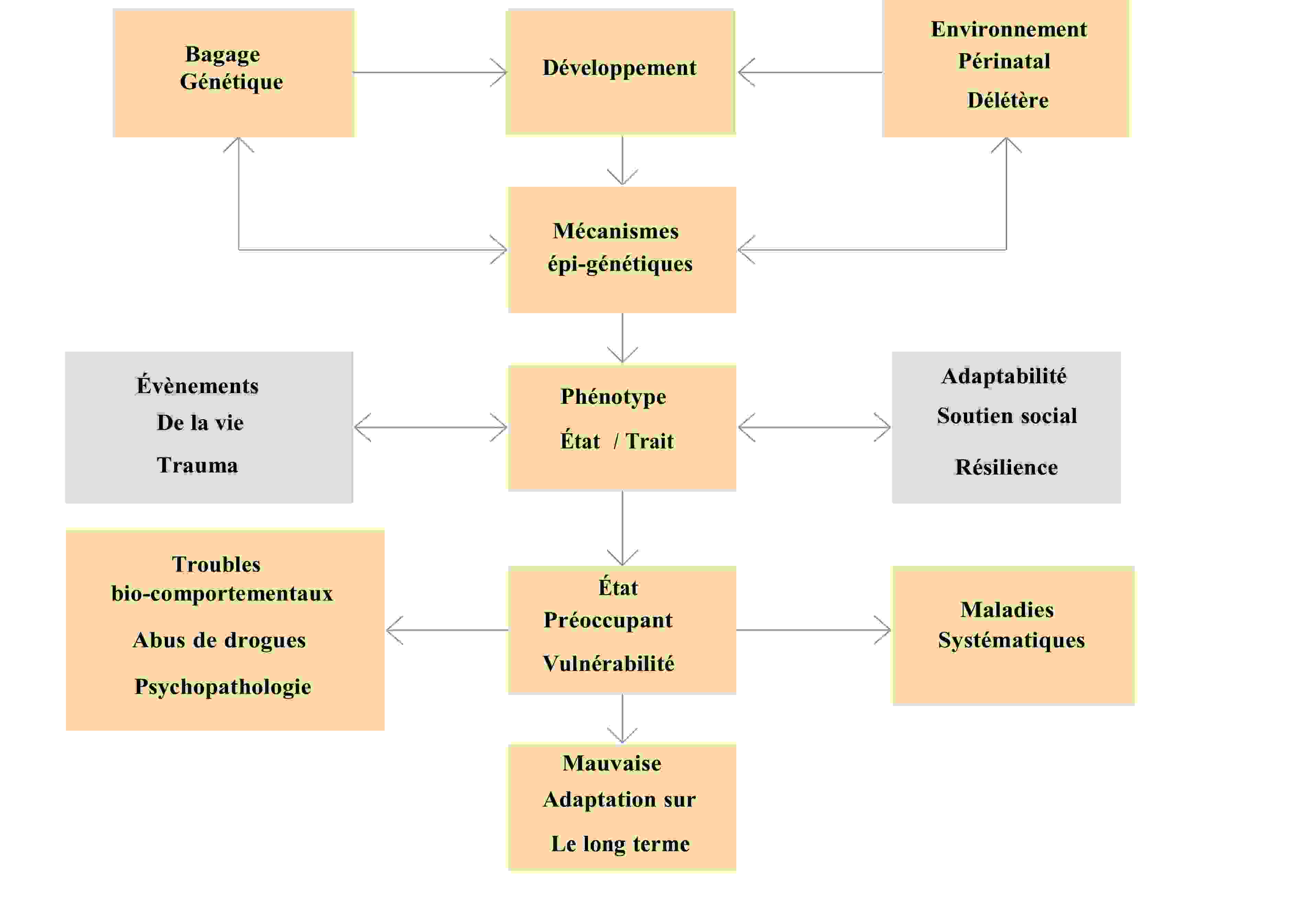
Biopsychosocial modeling in psycho-behavioral disorders and addictive (George F. Koob, Michel Le Moal., 2005):
Oral Session 2:
- Place of Citicholine and Neuroregulators in prevention, reduction of sequelae neurological and morbidity and mortality.
Title: Place of Citicholine and Neuroregulators in prevention, reduction of sequelae neurological and morbidity and mortality.
Biography:
Lamirez Diasivi Nzuzi is working for the department of neurosurgery at Mont-Amba University Hospital Center (CHMA), University of Kinshasa.
Abstract:
Context:
Cerebral malaria, acute malarial encephalitis due to Plasmodium falciparum: is an acute brain injury whose outcome may be fatal can lead to polymorphic neurological sequelae: hemiplegia / hemiparesis, speech disorders (motor aphasia de Broca, Sensory aphasia of Wernicke), behavioral disturbances, cognitive impairment, blindness, secondary epilepsy. In Africa Sub-Saharan, and more particularly in the DRC, Neuropalaria, knows a high frequency of neurological lesions with a very high lethality and the seriousness of their repercussions on the fate of the children who are victims of it. The neuropathological severity of acute malarial cerebral aggression is correlated with the high parasite density, with the phenomena of sequestration and cytoadherence, the inflammatory process, the presence of the factors of bad prognosis or ACSOS, the diagnostic and therapeutic delay; and the antimalarials, do not modify the evolutionary process of neurological lesions and those of sequelae. An approach Neuroadapted therapy (Citicholine and neuroregulators) introduced in our patients, from the acute phase (from D0: in first 24 hours / first 6 hours +++ to 7 days), until the stabilization phase (D0- 30 days), allowed us to: Improve perfusion of the areas of ischemic brain suffering, regulation of cerebral metabolism (aerobic glycolysis +++) and reduction of cerebral edema (vasogenic, cytotoxic +++); delay the evolution of the destruction of the neuronal membrane and neuronal degeneration; limit and block ischemic cascades leading to neuronal necrosis; Improve the prognosis and dramatic rapid recovery, speech recovery and significant reduction in other neurological sequelae, but also death-mortality.
To date, acute malarial encephalitis should be considered in mind as a normotensive ischemic stroke. post-infectious, until proven guilty, in the light of the neuroanatomo-clinical correlation, of the neurophysio- pathologies induced in acute and secondary cerebral aggression.
Goal:
Management of acute malarial encephalitis and its acute complications, and to propose a Neuroadapted therapeutic approach, by demonstrating the action of Citicholine and neuroregulators on Broca's area.
Methodology:
A serial study of cases admitted to the Emergency and Neuropediatrics Department for acute malarial encephalitis complicated by aphasia de Broca and other neurological sequelae.
Results
In the absence of certain medical files available and in the insufficiency of clinical and para-clinical data found in certain records, of the 30 patients registered for acute malarial encephalitis complicated by neurological deficits during the period of March 2021, we describe that two cases of Broca's Aphasia on Acute Malarial Encephalitis in two patients born and residing in DRC, Kinshasa. The first case; a 9-year-old male child admitted to the neuropediatric emergency room for tonic-clonic seizures and headaches, in his antecedents, no notion of previous seizure episode, no convulsors and epileptics in the family. Treatment received elsewhere, Quinine, Ciprofloxacin and Diazepam; In whom we note mainly at physical examination, Heart rate at 140 bpm, Respiratory rate at 40 cpm, Temperature at 38 ° C, Coma with convulsions
Tonic-clinical, febrile on palpation, colored eyelid conjunctivae and anicteric bulbar conjunctiva, an abdomen not bloated, sensitive to medium ureteral points and without organomegaly, Deep coma, Soft neck and no signs of neuro-irritations meningeal, isocoric and reflective pupils. On paraclinical examination, Hb at 12 g / l, occasional glycemia at 109 mg / dl, GE: Tropho +++, GB: 16000 elt and FL: N60% L40%; Widal (TH: 1/160, TO: 1/160), Blood ionogram, CT-brain scan and emergency EEG not performed, a treatment was initiated: made of injectable Artesunate (H0-H72), Oritaxim, Amikacin, Ciprofloxacin, a maintenance infusion :( SG5% + electrolytes + Nootropyl + Azantac) and feeding by gavage. The evolution would be marked on D5-D7 by an awakening initiated with Brocas motor aphasia, right hemiparesis, CT scan of the brain, performed: Left frontal hypodensity zone. Under Citicholine(Somazina) and Neuroregulators (Gamalate B6, Surmenalite), resumption of language 24 hours later, with end of tremors (impairment of central gray nuclei) under Artane ½ tablet for 7 days with a good spectacular development. File close and exit authorized with Trausan, Surmenalite and Gamalate B6 for 1 month; an appointment in 1 month with a cerebral CT-scan control.
The second case; she is a 27-year-old patient, admitted for temporo-spatial disorientation and headache. contributory, in whom the clinical examination notes a BP: 158/87 mm Hg, HR: 112bpm, FR: 24 cpm, patient with temporal disorientation spatial, EG altered by suffering mine, Colored eyelid conjunctiva and bulbar anicteric, on normal gynecological examination, on neurological examination; flexible neck and no signs of neuro-meningeal irritation, isocoric and reflective pupils. At the exam paraclinical; GE: Tropho +; incidental blood sugar: 112 mg / dl, Hb: 12 g / l, ESR: 60mm / H, GB: 12200elt, FLN62% L38%, Urinary sed (GB: 5-10 / elt, EC: 5-10 / elt), treatment with Artesunate, promethazine, ceftrin plus. The evolution was marked by a motor aphasia of Broca, a few hours after admission, a cerebral CT scan was urgently requested, not carried out given the financial situation patient, and she was on citicholine (Somazina) as a continuous infusion with antioxidants (VIT C, VIT E) in emergency, neurosedation with phenobarbital. On day 1 of hospitalization, i.e. 24 hours of hospitalization later, we observed the resumption of speech with temporo-spatial orientation, and vital signs in physiological norms. File close and exit authorized with Somazina tablet, Gamalate B6, Overmenalitis for 1 month.
Conclusion
Before any case of acute malarial encephalitis (cerebral malaria), it is of interest to add the neuroregulatory therapeutic regimen; improving the prognosis (rapid recovery), preventing the occurrence of neurological complications often irreversible and reduced morbidity and mortality. And Antimalarials, do not modify the evolutionary process of destruction neuronal and neurological sequelae.
Oral Session 3:
- Relationship between obesity and cognitive functions among medical students of International University of Africa 2019-2020
Title: Relationship between obesity and cognitive functions among medical students of International University of Africa 2019-2020
Biography:
Humeda Suekit is working as a Associate Professor at Azaiem Al-Azhari University, he is also the president of the Sudanese Obesity Organization.
Abstract:
Background: obesity is classified as chronic and severe disease in developed and developing countries with increasing prevalence worldwide. Obesity is associated with many non-communicable diseases such cardiovascular diseases; diabetes; musculoskeletal disorders; some cancers, respiratory problems and cognitive disorders. The relationship between obesity and impaired cognitive functions remains doubtful. The aim of this study was to determine the relationship between body mass index (BMI) and cognitive function.
Subjects and methods: This was observational descriptive cross section study and included all medical students at International University of Africa (IUA). Two hundred and ninety seven students were selected by stratified random sampling. For each student weight and height were measured and BMI was calculated. The cognitive function was assessed using modified mini-mental test which includes tests of orientation, registration, attention, calculation, recall, and visual- spatial skills. Data was analyzed using SPSS version 24 program. Descriptive data were presented as means+/- SD or frequencies. The relationship between BMI and cognitive function analyzed using ANOVA test. P value < 0.05 considered significant.
Results: The average age of students was 20.9 ± 1.9 years. The prevalence of obesity among medical students was 8.4%. Obesity had no significant relationship with gender or nationality. The average score of mini-mental test was 1.6 ± 0.7.
Female students had lower minimental score compared to males (P=0.05). There was no significant correlation between BMI and impaired cognitive function.
Conclusion: Obesity has no significant correlation with impaired cognitive function; however, cohort studies are necessary to investigate this relationship.




